Tpa Clot Treatment 3,3/5 5904 reviews
Generic Name: alteplase (AL te plase)
Brand Name:Activase, Cathflo Activase
Dosage Forms: injectable powder for injection (2 mg); intravenous powder for injection (100 mg; 50 mg)
What is alteplase?
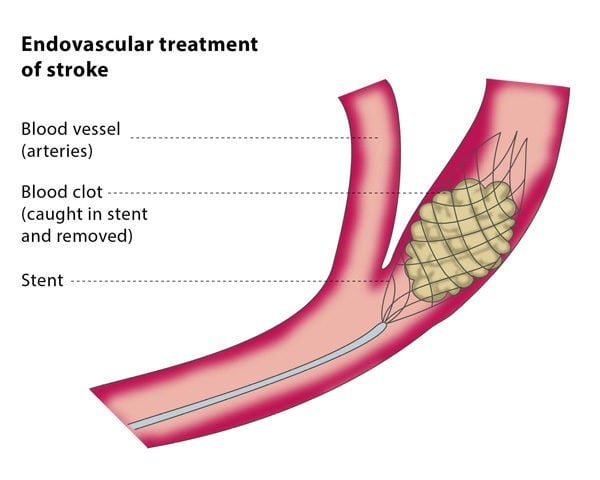
This image shows how applying clot-dissolving drugs like tPA directly to a blockage (intra-arterial thrombolytic therapy) or removing the clot with a special device can restore blood flow to the brain. This image shows how applying clot-dissolving drugs like tPA directly to a blockage (intra-arterial thrombolytic therapy) or removing the clot with a special device can restore blood flow to the brain.
Alteplase is a thrombolytic (THROM-bo-LIT-ik) drug, sometimes called a 'clot-busting' drug. It helps your body produce a substance that dissolves unwanted blood clots.
Alteplase is used to treat a stroke caused by a blood clot or other obstruction in a blood vessel. Alteplase is also used to prevent death from a heart attack (acute myocardial infarction).
Since tPA dissolves blood clots, there is risk of hemorrhage with its use. Administration criteria. Use of tPA in the United States in treatment of patients who are eligible for its use, have no contraindications, and arrival at the treating facility less than 3 hours after onset of symptoms, is reported to have doubled from 2003 to 2011. If you get to the hospital within 3 hours of the first symptoms of an ischemic stroke, you may get a type of medicine called a thrombolytic (a “clot-busting” drug) to break up blood clots. Tissue plasminogen activator (tPA) is a thrombolytic. TPA improves the chances of recovering from a stroke.
Alteplase is also used to treat a blood clot in the lung (pulmonary embolism).
Alteplase is also used to dissolve blood clots that have formed in or around a catheter placed inside a blood vessel. This improve the flow of medicines injected in through the catheter, or blood drawn out through the catheter.
Alteplase may also be used for purposes not listed in this medication guide.
Important Information
Alteplase increases your risk of severe or fatal bleeding, especially from a surgical incision, or from the skin where a needle was inserted. Seek emergency help if you have any bleeding that will not stop.
Before taking this medicine
You should not be treated with alteplase if you are allergic to it, or if you have:
active bleeding inside your body;
a brain tumor or aneurysm (dilated blood vessel);
a history of head injury or surgery on your brain or spinal cord within the past 3 months; or
severe or uncontrolled high blood pressure;
a bleeding or blood clotting disorder such as hemophilia;
bleeding inside your brain (if you are receiving alteplase to treat a stroke); or
a recent history of stroke (if you are receiving alteplase for pulmonary embolism).
Tpa Clot Treatment Definition
If possible before you receive alteplase, tell your doctor if you have ever had:
any type of stroke;
bleeding in your brain, stomach, intestines, or urinary tract;
high blood pressure;
heart problems;
an infection of the lining of your heart (also called bacterial endocarditis);
a serious injury or major surgery;
severe bruising or infection around a vein where an IV was placed;
an organ biopsy;
eye problems caused by diabetes;
liver or kidney disease; or
if you are pregnant or breastfeeding.
In an emergency situation it may not be possible to tell your caregivers if you are pregnant or breast-feeding. Make sure any doctor caring for your pregnancy or your baby knows you have received alteplase.
How is alteplase given?
Alteplase is given as an infusion into a vein. A healthcare provider will give you this injection.
Alteplase is usually given within 3 hours after the first signs of stroke or heart attack symptoms. Your breathing, blood pressure, oxygen levels, and other vital signs will be watched closely.
You will also be watched closely for several hours after receiving alteplase, to make sure you do not have an allergic reaction to the medication.
When used to clear blood clots from a catheter, alteplase is given in 1 or 2 doses.
Your doctor may prescribe a blood thinner or other medication to help prevent future blood clots. Carefully follow all dosing instructions. These medications can make it easier for you to bleed, even from a minor injury.
What happens if I miss a dose?
Because you will receive alteplase in a clinical setting, you are not likely to miss a dose.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid after receiving alteplase?
Ask your doctor before taking aspirin or ibuprofen (Motrin, Advil) shortly after you have received alteplase. These medications can increase your risk of bleeding.
Avoid activities that may increase your risk of bleeding or injury. Use extra care to prevent bleeding while shaving or brushing your teeth.
Alteplase side effects
Get emergency medical help if you have signs of an allergic reaction:hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Alteplase increases your risk of bleeding, which can be severe or fatal. Call your doctor or seek emergency medical attention if you have bleeding that will not stop. Bleeding may occur from a surgical incision, or from the skin where a needle was inserted during a blood test or while receiving injectable medication. You may also have bleeding on the inside of your body, such as in your stomach or intestines, kidneys or bladder, brain, or within the muscles.
Call your doctor or get emergency medical help if you have signs of bleeding, such as:
sudden headache, feeling very weak or dizzy;
bleeding gums, nosebleeds;
easy bruising;
bleeding from a wound, incision, catheter, or needle injection;
bloody or tarry stools, coughing up blood or vomit that looks like coffee grounds;
red or pink urine;
heavy menstrual periods or abnormal vaginal bleeding; or
sudden numbness or weakness (especially on one side of the body), slurred speech, problems with vision or balance.
Also call your doctor at once if you have:
chest pain or heavy feeling, pain spreading to the jaw or shoulder, nausea, sweating, general ill feeling;
swelling, rapid weight gain, little or no urination;
severe stomach pain, nausea, and vomiting;
darkening or purple discoloration of your fingers or toes;
very slow heartbeats, shortness of breath, feeling light-headed;
sudden severe back pain, muscle weakness, numbness or loss of feeling in your arms or legs;
increased blood pressure--severe headache, blurred vision, pounding in your neck or ears, anxiety, nosebleed; or
pancreatitis--severe pain in your upper stomach spreading to your back, nausea and vomiting.
Bleeding is the most common side effect of alteplase.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
What other drugs will affect alteplase?
Tell your doctor about all your other medicines, especially:
any medication used to treat or prevent blood clots;
a blood thinner (heparin, warfarin, Coumadin, Jantoven); or
NSAIDs (nonsteroidal anti-inflammatory drugs)--aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve), celecoxib, diclofenac, indomethacin, meloxicam, and others.
This list is not complete. Other drugs may affect alteplase, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2021 Cerner Multum, Inc. Version: 3.01.
More about alteplase
- During Pregnancy or Breastfeeding
Consumer resources
Other brands:Activase, Cathflo Activase
Professional resources
Related treatment guides
After suffering an ischemic stroke, and only a short time after symptoms began, tPA may be used.
© Zerbor Dreamstime
When a blood clot is stopping blood flow to the brain, a powerful clot-busting medication called tPA is used to dissolve the clot and restore blood flow. The drug must be given within 4½ hours after the onset of symptoms, or the risk of causing unwanted bleeding may outweigh the benefit. The earlier tPA is administered within that time period, the better the chances of a favorable outcome.
Tpa Clot Treatment Protocol
Knowing a patient’s vital signs, and armed with the results of a CT scan, ECG, blood tests, and history of stroke symptoms including time of onset, a physician can make a diagnosis. If the diagnosis is ischemic stroke, and only a short time has passed since symptoms began, tPA may be used.
Standard Treatment: tPA to Dissolve the Blood Clot
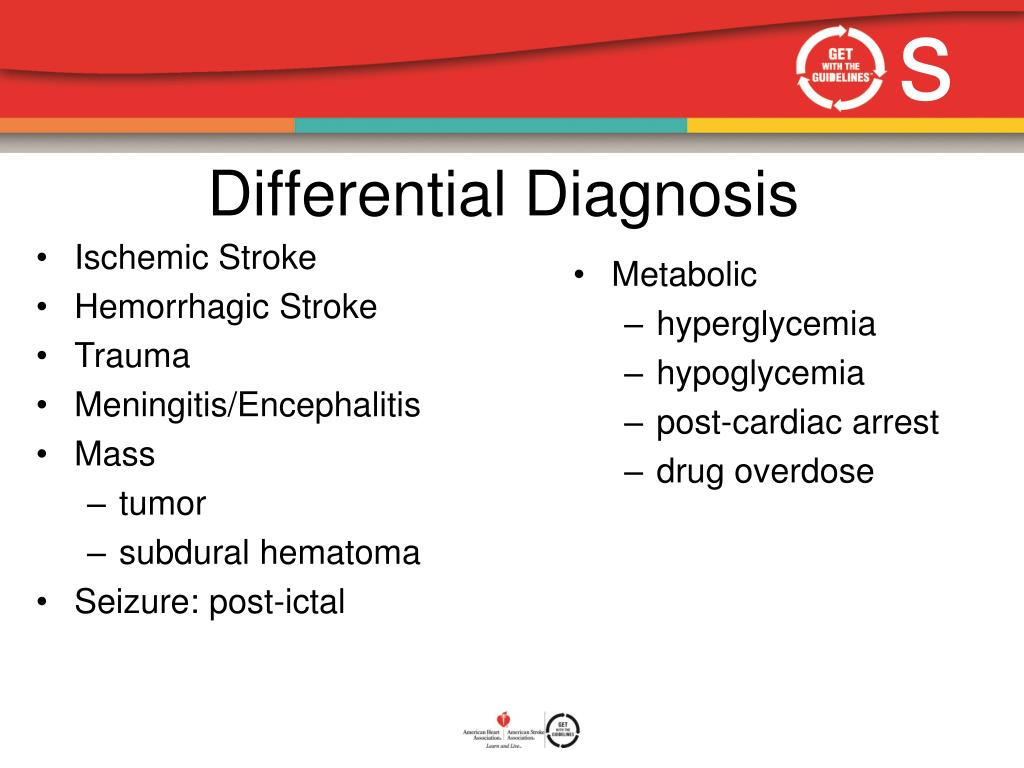
The technique for treating blood clots causing stroke is called intravenous thrombolysis—in lay terms, “clot-busting.” Thrombolysis is the combination of two Greek words, “thrombus,” meaning blood clot, and “lysis,” meaning to dissolve or break apart. The body has a natural mechanism for doing this through proteins that circulate in the blood. One of these is plasminogen, an inactive protein that the body converts to plasmin, an enzyme that breaks apart and dissolves blood clots. To make this conversion, another enzyme called tissue plasminogen activator (tPA) is required.
Blood clotting is a dynamic process. Fibrin filaments act like nets to trap red blood cells and stop the bleeding. As fibrin filaments form, tPA in the serum of the trapped blood begins to adhere to the fibrin, converting plasminogen to plasmin. Plasmin attacks the fibrin filaments, dissolving the net and breaking up the blood clot.
Blood clots are broken apart by plasmin as they form. So long as there is sufficient stimulus for blood to clot, clots will form faster than plasmin can break them apart. When the stimulus vanishes, the blood clot eventually breaks apart and disappears. The objective of thrombolytic therapy is to accelerate the removal of a blood clot by enhancing the conversion of inactive plasminogen to clot-busting plasmin.
Emergency Medical Treatment for Stroke
The use of tPA is so effective in treating acute ischemic stroke that it is used in emergency departments throughout the country. Unfortunately, only about five percent of patients who qualify for the treatment receive it. One reason is failure to arrive at the hospital within the recommended treatment window of 4.5 hours.
While several tPA drugs can be used to break up heart attack-causing blood clots in the coronary arteries, only one is approved for the treatment of ischemic stroke: alteplase (Activase). It is given by intravenous infusion. About 10 percent of the entire dose is given at one time (bolus), with the remaining 90 percent infused over an hour.
Initially, it was thought alteplase had to be administered within three hours of stroke onset. But when clinical trials showed the drug was safe and effective for a longer period of time, the American Heart Association/American Stroke Association (AHA/ASA) endorsed expanding the treatment window to 4.5 hours. The drug label says that risks are increased when the drug is used in patients over age 75, and its effectiveness in those over age 80 has not been established. But in 2015, the AHA/ASA gave a positive recommendation to tPA use in older patients, acknowledging that risk may be increased, but that it does not outweigh the potential benefit in increasing the likelihood of remaining independent three months after a stroke.
The AHA/ASA continues to emphasize that results are better when patients are treated earlier. Patients who receive the therapy within 90 minutes have a better outcome than those who receive it later, even if within the allowed time period. For every 30 minutes that pass before blood flow is restored through a blocked artery, the probability of a good recovery drops by about 10 percent.
Know the Risks
A danger of thrombolytic therapy is the possibility of unwanted bleeding. Clot-busting drugs cannot tell the difference between a “bad” clot that prevents blood flow to the brain cells and a “good” clot that has been formed to stop blood flow from a ruptured intracranial artery. If the drug breaks down a good clot, a hemorrhagic stroke can occur. Despite careful dosing, intracranial hemorrhage occurs in some patients who receive alteplase. Nevertheless, in appropriately selected patients, the benefits far outweigh this potential complication.
Tpa Blood Clot Treatment
When It’s Too Late for tPA
For patients diagnosed with ischemic stroke after the treatment window has passed, no medication to restore blood flow has been proven effective. However, some of these patients may benefit from mechanical removal of the clot with a catheter-based device up to six hours after stroke onset.